US Markets
Wednesday, August 30th, 2023 11:44 am EDT
Medicare is set to negotiate prices for 10 different drugs with manufacturers in a bid to make those costly treatments more affordable for older Americans – a process the pharmaceutical industry fiercely opposes.
But analysts say the drug price talks will likely have a muted financial impact on manufacturers, at least for this first round of prescription medicines.
That’s because other factors are already expected to weigh on the revenue and profits of the drugs on the list, which could minimize any negative impact from lower negotiated prices that are set in place. For example, many of the drugs are already facing strong competition from other branded medications or patent expirations in the coming years that will open the market to generic alternatives.
More broadly, some of the drugs on the list aren’t significant contributors to their company’s business in the first place.
“The commercial impact of negotiations appears limited in the near term for this initial list of drugs,” Mara Goldstein, managing director of Mizuho Securities, told CNBC.
That could change in future rounds of negotiations, analysts say.
The Biden administration unveiled the much-awaited list of drugs Tuesday, officially kicking off a lengthy negotiation process that will end in August 2024. The reduced prices won’t go into effect until January 2026.
The list names drugs with the highest spending for Medicare Part D, which covers prescription medications, from June 2022 to May 2023. That includes blood thinners from Bristol-Myers Squibb and Johnson & Johnson, and diabetes drugs from Merck and AstraZeneca.
However, there’s a chance that the negotiated prices will never actually go into effect. Several drugmakers, including a handful whose medications are on the list, have filed lawsuits in different federal courts seeking to stop the negotiations. That could set up split appellate court decisions and fast-track the dispute to the Supreme Court.
Meanwhile, the U.S. Chamber of Commerce, one of the largest lobbying groups in the country, is seeking a preliminary injunction to halt negotiations before Oct. 1. That’s the same day drugmakers have to sign agreements to participate in the negotiations. It’s unclear whether that effort will be successful.
Patent expirations, branded competition
New negotiated prices in 2026 may have a minimal financial impact on drugs already expected to see revenue and profits decline due to upcoming patent expirations and branded competition.
For example, Merck’s Type 2 diabetes drug Januvia could lose exclusivity in mid-2026 – only a few months after the negotiated prices go into effect. Goldstein said she expects to see 90% of the volume from Januvia go to cheaper generic competitors within the first few months of the patent expiration.
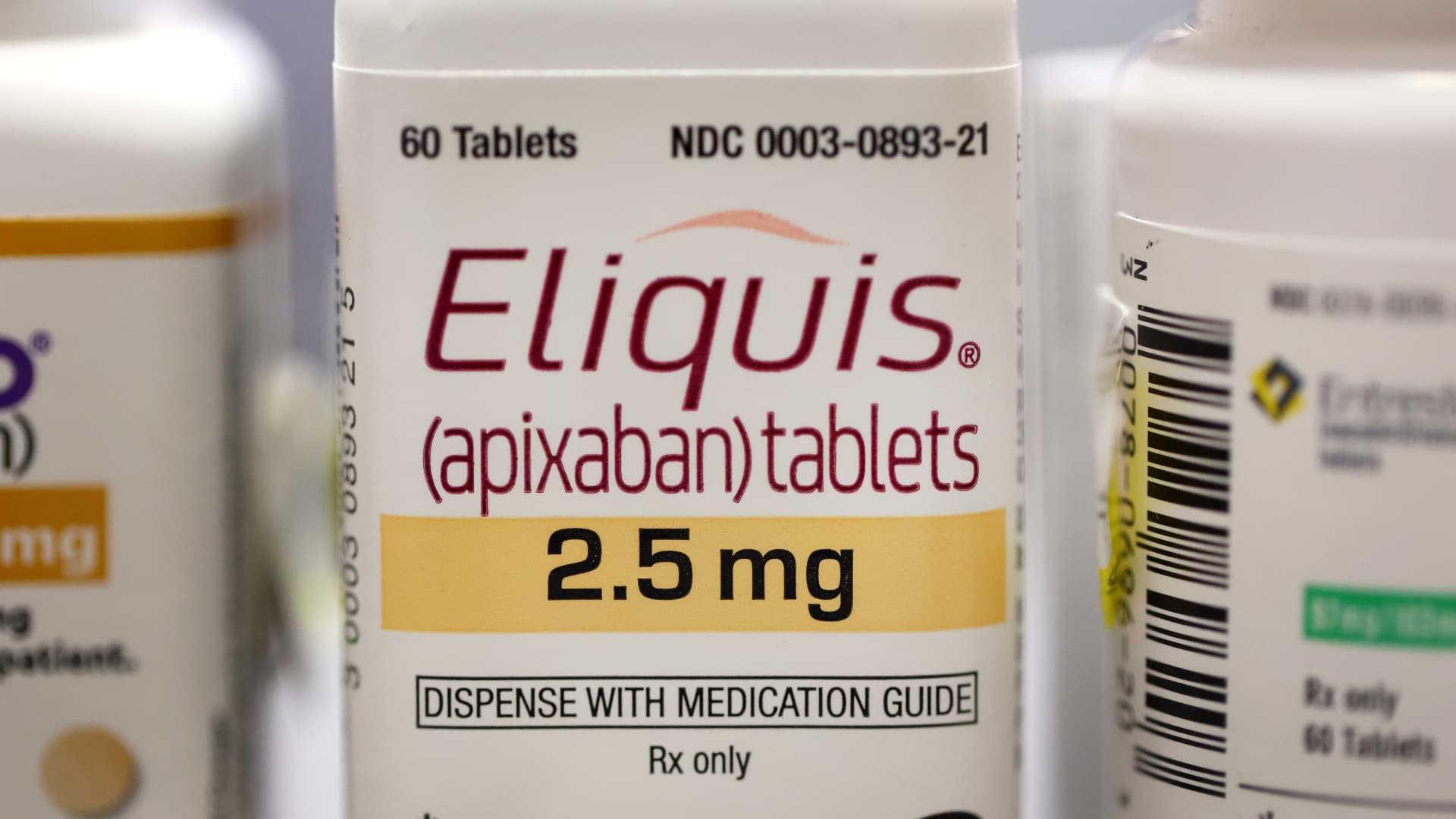
- Eliquis, made by Bristol-Myers Squibb, is used to prevent blood clotting, to reduce the risk of stroke.
- Jardiance, made by Boehringer Ingelheim, is used to lower blood sugar for people with Type 2 diabetes.
- Xarelto, made by Johnson & Johnson, is used to prevent blood clotting, to reduce the risk of stroke.
- Januvia, made by Merck, is used to lower blood sugar for people with Type 2 diabetes.
- Farxiga, made by AstraZeneca, is used to treat Type 2 diabetes.
- Entresto, made by Novartis, is used to treat certain types of heart failure.
- Enbrel, made by Amgen, is used to treat rheumatoid arthritis.
- Imbruvica, made by AbbVie, is used to treat different types of blood cancers.
- Stelara, made by Janssen, is used to treat Crohn’s disease.
- Fiasp and NovoLog, insulins made by Novo Nordisk
“So, doing any negotiating for Januvia today seems like kind of a moot point since it will be losing exclusivity in 2026 and seeing this decline due to generic competition,” she told CNBC.
The same is true for AstraZeneca’s Type 2 diabetes drug Farxiga, which will lose exclusivity in 2026, and other drugs on the list with later patent expirations, according to a note from David Risinger, an analyst at Leerink Partners.
Johnson & Johnson’s blood thinner Xarelto and Novartis’ heart failure drug Entresto are both expected to lose exclusivity in 2027. That means the companies may only feel the impact of negotiated prices for their drugs for about one year before generic competition minimizes the effect of that, Risinger wrote.
Eliquis, a blood thinner from Bristol-Myers Squibb and Pfizer, is slightly more exposed to the impact of negotiated prices since its patent expires in 2028. But that risk will likely be manageable.
“We think Bristol/Pfizer could take a low-mid single-digit hit to their respective 2026 revenue … due to Eliquis negotiation,” Bank of America analyst Geoff Meacham said in a research note Tuesday, adding that the effect of negotiated prices will be limited to 2026 and 2027.
Branded competition is another factor that could mute the impact of negotiated prices, Meacham added.
For example, AbbVie‘s blood cancer drug Imbruvica could see steep declines before its negotiated price goes into effect in 2026, largely due to “competitive erosion” from similar treatments like AstraZeneca’s Calquence and Beigene‘s Brukinsa, according to Meacham.
Competition between similar branded medications has already resulted in rebates and discounts paid to Medicare Part D for some of the drugs on the list. That raises questions about how much lower of a price Medicare can negotiate.
Cantor Fitzgerald analyst Louise Chen also emphasized that many of the drugs on the list aren’t the key growth drivers of their companies in the first place. That means any decline in a drug’s sales and profits may do little to affect the company’s overall business and stock.
For example, Merck’s Januvia is a smaller revenue and earnings contributor than other drugs in the company’s pipeline, such as its blockbuster cancer drug Keytruda or HPV vaccine Gardasil. Januvia generated $4.5 billion in revenue last year, while Keytruda raked in $21 billion.
The next negotiations could be different
But Chen said that could change in 2028 and beyond, when negotiations will also start targeting drugs in Medicare Part B.
Part B covers more specialized medications that are administered by doctors or other health care providers rather than pharmacies. That includes Keytruda and other biologic medications, which are created using living cells or organisms.
“When we get to more biologics, the impact is going to be a lot more significant because those products are much more expensive and impact the earnings and growth of these companies a lot more,” Chen said.
Mizuho’s Goldstein also added that drug price negotiations will likely have more of a long-term impact on companies, even if it “certainly feels muted right at this moment.”
Over time, negotiations could change a company’s drug development strategy.
Negotiated prices prevent companies from maintaining pricing power over a treatment, so “the thought process is that continuing to reinvest in a drug to add additional indications has a less compelling return,” according to Goldstein. Expanding indications refers to using a drug to treat a different disease.
This post has been syndicated from a third-party source. View the original article here.